
Maleeha Qazi, PhD
MD Candidate, University of Toronto, Canada
In December 2019, the first cases of patients with pneumonia-like viral illness were identified in Wuhan, China. Subsequently, a novel human-infecting coronavirus (termed SARS-CoV-2) was identified as the causative agent for the illness1. Since then 210 countries and territories have reported cases of COVID-19 (COronaVIrus Disease-2019), with global cases topping 4 million and close to 300,000 confirmed deaths (WHO COVID-19 Situation Report – 112, 11th May 2020). With the COVID-19 pandemic raging across the globe, multiple avenues of treatments are being developed and tested for efficacy against SARS-CoV-2 pathogen. As of yet, there are no universal cures against COVID-19 and the search for an effective vaccine still continues.
What is COVID-19?
COVID-19 is the official name assigned by the World Health Organisation (WHO) to the disease caused by SARS-CoV-2 virus. SARS-CoV-2 belongs to a large family of viruses called coronaviruses that are believed to have been originated in bats2. Through genetic mutations, these viruses are thought to have spilled over from bats to other animals, and subsequently mutated further to infect humans. Over the past 20 years, two such coronaviruses have caused highly pathogenic outbreaks in humans: 2002 severe acute respiratory syndrome (SARS) outbreak caused by SARS-CoV and 2012 Middle East respiratory syndrome (MERS) outbreak caused by MERS-CoV.
SARS CoV-2,like its predecessors, infects human cells found in the respiratory systems, leading to common symptoms like fever, cough, and shortness of breath. However, in severe cases, the disease progresses to pneumonia and multi-organ failure, ultimately leading to death. The rapid spread of the SARS CoV-2 is what has set it apart from other coronaviruses, leaving nations across the world scrambling for ways to reduce its transmission. Furthermore, there are no known treatments to either prevent or treat the disease, with disease management limited to supportive care3. As we all watch the pandemic affecting people close to us, we are left to wonder when a treatment will become available to cure us of this disease?
Disease and its cure – the Islamic perspective
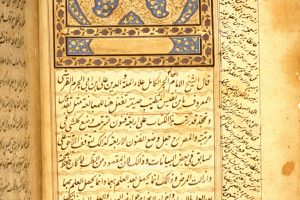
The Holy Qur’an explains that Allah the Almighty is the source of health for those who are sick as Prophet Abraham (as) told his people, ‘And when I am ill, it is He Who restores me to health‘ (Holy Quran, 26:81). This injunction is further corroborated by a Hadith of the Holy Prophet Muhammad (sa) as is narrated by Abu Hurairah (ra), ‘There is no disease that Allah has created, except that He also has created its treatment.’ (Sahih al-Bukhari, 5678, Book 76, Hadith 1). While human effort result in the discovery of new treatments for diseases, it is Allah the Almighty in His infinite compassion and grace Who has given mankind the intellect to support these endeavours and He guides those who seek them to fulfilment. Allah’s compassion for His creation provides hope that while the situation maybe dire, He will provide the necessary cures. Though, human effort is indeed needed which is channeled towards research efforts that attempt to better understand human diseases and use that knowledge in the development of treatments. The Fifth Caliph and worldwide Head of the Ahmadiyya Muslim Community, Hazrat Mirza Masroor Ahmad (aba) clarified the purpose of these efforts in his message to students conducting research during his 2016 tour of Germany, ‘Every person is going to die one day, however it is very important that we use our brains to try and find cures for the illness and ailments that cause so much suffering and to try and improve the quality of people’s lives. This is the essence and true spirit with which research should be conducted.’ (From ‘A Personal Account’ by Abid Khan — Huzoor’saa tour of Germany 27th Aug – 10th Sept 2016 — Part 1, under ‘Student classes with Huzooraa page 20-21).
With this hope that a cure, God willing, will be found, we relate some of the efforts that are being performed around the world for curing COVID-19. Furthermore, millions around the world are praying for the success of these scientists — it is this combination of effort and prayer that attracts the mercy of Allah.
Repurposing Drugs
Although a vaccine against SARS-CoV-2 will serve as the most effective strategy for long-term infection control, repurposing of drugs designed to treat other conditions may offer quicker solutions to control the pandemic. While the treatment landscape for SARS-CoV-2 is rapidly evolving, a number of candidate therapies are already being evaluated in human patients by both government-funded organizations (for example NIH in USA, NIHR in UK, and CIHR in Canada) and pharmaceutical companies. Here we describe some of the current therapies being tested for the treatment of SARS-CoV-2 and detail the absolute need for a vaccine against SARS-CoV-2 to control the COVID-19 pandemic.
Chloroquine
One of the promising agents touted widely in the media is the use of chloroquine and hydroxychloroquine for the treatment of COVID-19. These two drugs are most commonly used for treating malaria and autoimmune conditions, including lupus and rheumatoid arthritis. While malaria (caused by a single celled Plasmodium ) is biologically very different to coronavirus, the drugs have different effects on human cells which can disrupt the ability of pathogens to infect cells and also limit their ability to replicate4. Hydroxychloroquine was first tested as a possible treatment against coronavirus infection back in 2002, after the emergence of SARS outbreak5,6. At that time, the drug was only tested in laboratory cell cultures and no randomized control studies were conducted in actual patients.
Similar to its effects against SARS-CoV, chloroquine/hydroxychloroquine has now also shown promise against SARS-CoV-2 in laboratory settings7–9. Early clinical studies seemed to suggest it could be quite effective in patients infected with SARS-CoV-210, which created much enthusiasm that it could be used as a treatment for COVID-19 patients. These were preliminary observational studies and were not the high-quality randomized trials that are typically used to assess effectiveness. Despite the limited clinical data, the US Federal Drug Administration approved the emergency use of hydroxychloroquine in COVID-19 patients. Soon after, conflicting evidence for the efficacy and safety of these drugs emerged, pressing the need for randomized controlled trials. In fact, the first randomized controlled trial of hydroxychloroquine for the treatment of SARV-CoV-2 infection that enrolled 150 patients did not show any effectiveness of the drug11. Currently, National Institute of Health (NIH) has started a blinded, placebo-controlled randomized clinical trial (NCT04332991), which aims to enroll more than 500 adults to further elucidate whether treatment with hydroxychloroquine can in fact help COVID-19 patients beyond standard hospital care. Similar clinical trials have also been undertaken in Canada, Australia and in multiple European countries. However, until conclusive evidence in support of chloroquine/hydroxychloroquine becomes available, the use of these compounds is being recommended only in an emergency situation for patients with severe COVID-19 symptoms while carefully considering the risks associated with this drug related to heart issues12–14.
Remdesivir
Remdesivir is a broad spectrum antiviral treatment (meaning it works against a range of diseases), that has shown positive signs in animal models for treating viruses like SARS-CoV , MERS-CoV, and MERS15. Remdesivir works by blocking the ability of viruses to replicate15. For this reason, researchers are interested in testing Remdesivir as a possible treatment for COVID-19. Early in the spread of COVID-19 this drug was used to treat patients with severe symptoms on compassionate grounds. A small study with a limited number of patients had promising results as 36 of 53 patients (68%) with severe symptoms showed clinical improvements15. A study with close to 300 patients with COVID-19 tested remdesivir in a randomized controlled trial and while the researchers noted a reduction in time to clinical improvement, no significant clinical benefit was associated with remdesivir treatment 16However, larger randomized controlled trial of this treatment are currently underway to comprehensively evaluate remdesivir efficacy in treatment of COVID-19. Gilead, the pharmaceutical company that developed Remdesivir, has started a Phase 3 clinical trial as of March 2020. Approximately 1,000 randomized patients have been enrolled from countries with high prevalence of COVID-19 to test the safety and efficacy of Remdesivir in patients with moderate symptoms of COVID-19 compared to standard-of-care17. Among the leading drug candidates, Remdesivir is considered to be the most promising18.
The above two drugs are some of the most popular ones that have gained attention in the recent weeks, but as highlighted above, both are not proven treatments. Without conclusive evidence, it is not clear whether these drugs will improve recovery for all patients or if they are even safe. This is why in late March, the World Health Organization (WHO), launched an extraordinary international initiative to test over a dozen different treatment combinations in the ‘SOLIDARITY’ trial18,19. The trial will test several drugs, such as chloroquine/hydroxychloroquine, Remdesivir, and others as trials go underway in different countries. All of the drugs are approved treatment for other diseases and are being essentially re-purposed for treating COVID-19. The aim is by bringing together clinical data from more than 100 countries, the SOLIDARITY trial can quickly recruit thousands of patients, coordinate efforts to analyze the results, and ultimately generate evidence that can rapidly inform health authorities across the world18.
Plasma Therapy – sharing the immunity
Drugs may be one option, but perhaps the treatment of COVID-19 may lie in something less pharmacological. One idea is to look towards the people who have beaten the virus i.e. the patients who have recovered from the disease. The answer may lie, quite literally, within their veins.
As with any infection, the human body responds by generating an immune reaction, that produces antibodies that can bind and neutralize the pathogen. In the case of COVID-19, such antibodies are generated against components of the SARS-CoV-2 virus that block the virus from binding to the human cells, prevent them from causing an infection. Once COVID-19 patients develop enough antibodies, they can fight off the virus and see improvements in their health. Importantly, this built-up immunity remains within recovered patients’ blood in case the virus reappears, and the antibodies need to be redeployed to attack the virus. One therapeutic hypothesis is that as more patients recover from COVID-19, it may be possible to transfuse the plasma (component of the blood that contains antibodies) from recovered patients into those who are suffering from severe COVID-19 infection. The recovered patients essentially share their immunity against SARS-CoV-2 infection helping others recover20.
While the idea may seem peculiar, it won’t be the first time a similar approach has been used. Plasma therapy was previously used during the 2002 SARS epidemic, various influenza pandemics (H1N1, H5N1) and against Ebola, demonstrating safety and effectiveness is certain cases21. A small series of patients (5 adult patients in the first study and 10 adult patients in the second study) have already been treated with plasma therapy for COVID-19, showing clinical improvement after plasma transfusion containing anti-SARS-CoV-2 antibodies from recovered patients’ donor blood21,22. While the results are encouraging, as with previous testing, the plasma therapy intervention has not tested on a wider scale in a randomized controlled trial. In addition, the characteristics of the donor, the dosing and timing of the therapy, and other aspects of care cannot be assessed with the current research. Lastly, as with any immune response to a pathogen, the strength of immunity can diminish with time and make the patient vulnerable to possible reinfection. Hence, even with a generation of a primary immune response against SARS-CoV-2, it is unknown whether recovered patients or those who receive plasma therapy remain completely immune and protected against future reinfections23. Researchers are now undertaking large-scale clinical trials to fully assess the utility of plasma therapy in improving clinical outcomes for COVID-19 positive patients without resulting in any adverse side-effects24.
SARS-CoV-2 antibodies – creating the immunity
Although the presence of neutralizing antibodies against SARS-CoV-2 can lead to clinical improvements in patients with COVID-19, plasma therapy can be limited by the availability of patients who have recovered, the ability of different medical centres to collect plasma and perform transfusions, and adverse events related to sharing of plasma from one person to another25. A similar but alternative option for treating patients with neutralizing anti-SARS-CoV-2 antibodies is to produce these antibodies in another organism – the quintessential research mouse or even a llama. Two recent studies have showed the production of anti-SARS-CoV2 antibodies in animal models that can be easily deployed for use in humans26,27. Using a special mouse model that can generate human antibodies rather than mouse antibodies, a group of Dutch researchers exposed mice to a specific part of the SARS-CoV-2 virus (termed an antigen) such that the mice generate an immune response in a manner similar to seen in humans26. Upon studying all the various human antibodies produced by the mice in response to SARS-COV-2 antigen, the researchers identified a potent antibody that could neutralize both SARS-CoV and SARS-CoV-2. Similarly, an international group of researchers from Germany, Belgium and the US were initially using llamas to develop small neutralizing antibodies against SARS-CoV and MERS-CoV viruses that can be administered via inhalers, much like those used for the treatment of asthma27. The researchers found that one of these neutralizing antibodies produced in llamas was also able to neutralize SARS-CoV-2 and can be mass produced in cell culture systems. It is worth noting that llamas belong to the camel family. While antibodies from both sources have only been tested in cell culture studies, they open a wide avenue for further development and production of these antibodies as therapeutics against COVID-19.
Vaccines – the end goal
All treatments, be they pharmacological or antibody-based, rely on people becoming sick before they receive any intervention. In medicine, a common idiom is that ‘prevention is better than a cure,’ and accordingly a vaccine provides the opportunity to stop the virus in its early infectious tracks. Since the genetic sequence for SARS-CoV-2 was first made available in early January, significant and rapid efforts have been undertaken to develop a vaccine against SARS-CoV-2.
Vaccines have been effective at preventing lethal infectious diseases such as polio, tetanus, measles and mumps to name a few and has even led to the eradication of smallpox28. A vaccine against viral infections is generally composed of a weakened virus (live or dead) or a component of the virus (termed antigen) such that injection with the vaccine elicits an immune response without causing a complete infection. As the immune system gets activated, it starts producing neutralizing antibodies in the same manner as it would if the host was infected by the real virus. This induced immune response gives our cells the opportunity to retain this immune memory and consequently protect us from future infections for a period of time by quickly deploying to attack the virus.
The development of a vaccine is an arduous process that requires months of preclinical investigations, laboratory work to find good antigens that can generate an appropriate yet strong immune response, and showing that it can work in proof-of-principle animal studies29. Under current circumstances, many steps involved in vaccine development have been accelerated but challenges around proper antigen identification and design, mitigating potential adverse effects (such as an allergic reaction to the vaccine) and determining how long vaccine-induced immune memory lasts remain30. Currently, six candidate vaccines are in clinical trial stages, which test for safety and dosing of the vaccine, while over 70 vaccine candidates are in pre-clinical stages of testing. The majority of vaccines currently under development aim to induce neutralizing antibody production against parts of SARS-CoV2 virus that bind to the surface of human lung cells31. If the virus can’t bind or latch on to our cells, it will not be able to infect and replicate to cause any substantial harm.
The Pursuit of Excellence
COVID-19 pandemic has shown that we need the highest-level of evidence to decide which treatments are the most effective. While urgent situations may require that established drugs be given based upon limited evidence and on compassionate grounds (e.g., hydroxychloroquine in COVID-19), this, however, is not ideal. Research studies which are observational in nature are prone to bias and thus are not very reliable for determining effectiveness of a treatment. While it can seem exciting when some early results show promise, until they can be tested rigorously, it is possible the therapies are no better than supportive care. Sacrificing the rigour, standard, and quality of scientific research may expose patients to undue harm and pose strong ethical challenges for healthcare professionals32. Randomized controlled trials have been considered the gold standard33,34 for judging the benefit of treatment for more than 70 years in evidence-based medicine, and in COVID-19, it will also be the method of choice to find which treatment is the best. High quality randomized trials remove bias by randomly allocating patients in to two groups and thus any other factor that might affect them are equally distributed. In addition, a control arm allows for direct comparison of the effectiveness of any treatment against another or placebo. Therefore, with many more treatments being tested on a daily basis for the treatment and prevention of COVID-19, the answers to how researchers and clinicians will finally treat the patients and control COVID-19 spread will lie in high-quality randomized controlled clinical trials.
About the author: Maleeha Ahmad Qazi completed her PhD in biochemistry and biomedical sciences from McMaster University (Canada), where she was the recipient of Canadian Institute of Health Research doctoralship and Canadian Neuro-Oncology Young Investigator award for excellence in brain tumour stem cell research. She is currently a first year medical student at the University of Toronto with a clinical interest in neurosurgery and neuro-oncology to care for patients with primary and metastatic brain cancers. She also serves as the Editor-in-Chief for the University of Toronto Medical Journal, the oldest student-run peer reviewed journal in Canada. She is actively involved with the Ahmadiyya Muslim Women Association of Canada, focusing on mentorship for students pursuing STEM education.
References
1 Zhu N, Zhang D, Wang W, et al.A Novel Coronavirus from Patients with Pneumonia in China, 2019. New England Journal of Medicine2020; 382: 727–33.
2 Cui J, Li F, Shi Z-L. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol2019; 17: 181–92.
3 Advice for public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed April 27, 2020).
4 Slater AFG. Chloroquine: Mechanism of drug action and resistance in plasmodium falciparum. Pharmacology & Therapeutics1993; 57: 203–35.
5 Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R. Effects of chloroquine on viral infections: an old drug against today’s diseases. The Lancet Infectious Diseases2003; 3: 722–7.
6 Vincent MJ, Bergeron E, Benjannet S, et al.Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virology Journal2005; 2: 69.
7 Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. Journal of Critical Care2020; published online March 10. DOI:10.1016/j.jcrc.2020.03.005.
8 Liu J, Cao R, Xu M, et al.Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov2020; 6: 1–4.
9 Wang M, Cao R, Zhang L, et al.Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res2020; 30: 269–71.
10 Gautret P, Lagier J-C, Parola P, et al.Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. International Journal of Antimicrobial Agents2020; : 105949.
11 Tang W, Cao Z, Han M, et al.Hydroxychloroquine in patients with COVID-19: an open-label, randomized, controlled trial. medRxiv2020; : 2020.04.10.20060558.
12 ServickApr. 21 K, 2020, Pm 3:40. Antimalarials widely used against COVID-19 heighten risk of cardiac arrest. How can doctors minimize the danger? Science | AAAS. 2020; published online April 21. https://www.sciencemag.org/news/2020/04/antimalarials-widely-used-against-covid-19-heighten-risk-cardiac-arrest-how-can-doctors (accessed April 26, 2020).
13 Borba MGS, Val F de A, Sampaio VS, et al.Chloroquine diphosphate in two different dosages as adjunctive therapy of hospitalized patients with severe respiratory syndrome in the context of coronavirus (SARS-CoV-2) infection: Preliminary safety results of a randomized, double-blinded, phase IIb clinical trial (CloroCovid-19 Study). medRxiv2020; : 2020.04.07.20056424.
14 Giudicessi JR, Noseworthy PA, Friedman PA, Ackerman MJ. Urgent Guidance for Navigating and Circumventing the QTc-Prolonging and Torsadogenic Potential of Possible Pharmacotherapies for Coronavirus Disease 19 (COVID-19). Mayo Clin Proc2020; published online April 7. DOI:10.1016/j.mayocp.2020.03.024.
15 Grein J, Ohmagari N, Shin D, et al.Compassionate Use of Remdesivir for Patients with Severe Covid-19. New England Journal of Medicine2020; 0: null.
16 Wang Y, Zhang D, Du G, et al.Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. The Lancet2020; 0. DOI:10.1016/S0140-6736(20)31022-9.
17 Remdesivir Clinical Trials. https://www.gilead.com/purpose/advancing-global-health/covid-19/remdesivir-clinical-trials (accessed April 26, 2020).
18 Kupferschmidt K, Cohen J. Race to find COVID-19 treatments accelerates. Science2020; 367: 1412–3.
19 “Solidarity” clinical trial for COVID-19 treatments. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-clinical-trial-for-covid-19-treatments (accessed April 27, 2020).
20 Chen L, Xiong J, Bao L, Shi Y. Convalescent plasma as a potential therapy for COVID-19.The Lancet Infectious Diseases2020; 20: 398–400.
21 Duan K, Liu B, Li C, et al.Effectiveness of convalescent plasma therapy in severe COVID-19 patients. PNAS2020; published online April 6. DOI:10.1073/pnas.2004168117.
22 Shen C, Wang Z, Zhao F, et al.Treatment of 5 Critically Ill Patients With COVID-19 With Convalescent Plasma. JAMA2020; published online March 27. DOI:10.1001/jama.2020.4783.
23 ‘Immunity passports’ in the context of COVID-19. https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19 (accessed April 27, 2020).
24 Canada begins clinical trial of experimental COVID-19 treatment using plasma from recovered individuals. https://www.theglobeandmail.com/canada/article-canada-begins-clinical-trial-of-experimental-covid-19-treatment-using/ (accessed April 26, 2020).
25 Roback JD, Guarner J. Convalescent Plasma to Treat COVID-19: Possibilities and Challenges. JAMA2020; 323: 1561–2.
26 Wang C, Li W, Drabek D, et al.A human monoclonal antibody blocking SARS-CoV-2 infection. Nature Communications2020; 11: 2251.
27 Wrapp D, De Vlieger D, Corbett KS, et al.Structural Basis for Potent Neutralization of Betacoronaviruses by Single-Domain Camelid Antibodies. Cell2020; published online May 5. DOI:10.1016/j.cell.2020.04.031.
28 Plotkin S. History of vaccination. Proc Natl Acad Sci U S A2014; 111: 12283–7.
29 Leroux-Roels G, Bonanni P, Tantawichien T, Zepp F. Vaccine development. Perspectives in Vaccinology2011; 1: 115–50.
30 Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 Vaccines at Pandemic Speed. New England Journal of Medicine2020; 0: null.
31 Le TT, Andreadakis Z, Kumar A, et al.The COVID-19 vaccine development landscape. Nature Reviews Drug Discovery2020; published online April 9. DOI:10.1038/d41573-020-00073-5.
32 London AJ, Kimmelman J. Against pandemic research exceptionalism. Science2020; published online April 23. DOI:10.1126/science.abc1731.
33 Barton S. Which clinical studies provide the best evidence? BMJ2000; 321: 255–6.
34 Murad MH, Asi N, Alsawas M, Alahdab F. New evidence pyramid. Evid Based Med2016; 21: 125–7.



The article well written. As the proven medicens still not available for CV19 and the Scientist research is just aroud Allopathic findings.
The Question arises Wouldn’t be great if Sicence could expand the circle of research on a wider scale finding safe proven cure from Homeopathy and Herabl?